Are ICHRAs ACA Compliant?

ICHRAs allow businesses to meet their legal obligation to provide health insurance to their employees set by the Affordable Care Act (ACA).
What is the ACA Employer Mandate?
The Employer Mandate requires Applicable Large Employers to offer Minimum Essential Coverage to at least 95% their full-time employees and their children up to age 26.
The health coverage offered must be affordable and meet minimum value requirements.
Otherwise, the employer potentially faces penalties.
Who does the ACA Employer Mandate apply to?
Applicable Large Employers (ALEs)
An ALE is a business that employs 50 or more full-time employees or full-time equivalent employees (FTEs).
(Note: Part-time employees can be combined to represent full-time equivalent employees, which can push an employer over the 50-employee threshold.)
What are the ACA’s Affordability and Minimum Value requirements?
Health insurance coverage is considered affordable if an employee's share of the premium for employee-only coverage doesn’t exceed a certain percentage of their annual household income. This percentage is adjusted by the IRS annually. For 2025, the percentage is 9.02%.
A health insurance plan provides "Minimum Value" if it covers at least 60% of the total allowed cost of benefits. This means that the plan covers 60% of health costs, and the individual (i.e., employee) is responsible for the other 40% through a combination of deductibles, co-pays, and coinsurance.
For ICHRAs, this "Minimum Value" is actually higher. Silver Plans are used to calculate ACA Affordability. These plans cover 70% of the total allowed benefit costs.
ICHRA & the ACA Employer Mandate
ICHRAs meet ACA Employer Mandate requirements if the following three conditions are satisfied.
1. Only Qualified Health Plans (QHPs) are reimbursed.
One of the foundational ACA requirements is that insurance plans meet certain consumer protection standards. For an ICHRA to be considered compliant, reimbursements should only be for individual health insurance policies that qualify as a QHP.This ensures that the plans are robust, provide essential health benefits, and adhere to established limits on cost-sharing.
2. ICHRA contribution meets ACA Affordability standards.
While ICHRA allows employers to set reimbursement amounts, the ACA mandates that the coverage must be affordable for employees. Read our article about ACA Affordability for ICHRA to learn more.
3. Non-discrimination rules are followed.
With ICHRAs, employers can differentiate allowances based on specific employee classes, but they cannot discriminate within those classes based on health factors.
What happens if an employer fails to meet the ACA Employer Mandate?
Employers are at risk of penalties from the IRS. There are two primary penalties:
"No Offer" Penalty - Section 4980H(a)
This penalty is triggered if the ALE does not offer MEC to at least 95% of full-time employees and their dependents, and at least one full-time employee receives a premium tax credit through the Marketplace/Exchange.
"Inadequate Coverage" Penalty- Section 4980H(b)
This penalty applies if the ALE offers coverage, but it’s not affordable or does not provide minimum value, and at least one full-time employee receives a premium tax credit.
A penalty is incurred for each full-time employee that claims Premium Tax Credits from Healthcare.gov.
Venteur conducts extensive compliance reviews of all ICHRA plans that we administer to ensure full ACA compliance. Working with a different ICHRA administer and want to know whether your ICHRA is ACA compliant? Get in touch with us to conduct a compliance review.
You got questions, we got answers!
We're here to help you make informed decisions on health insurance for you and your family. Check out our FAQs or contact us if you have any additional questions.
Explore more related content
What is Venteur
Explore the best human-first Health Insurance platform
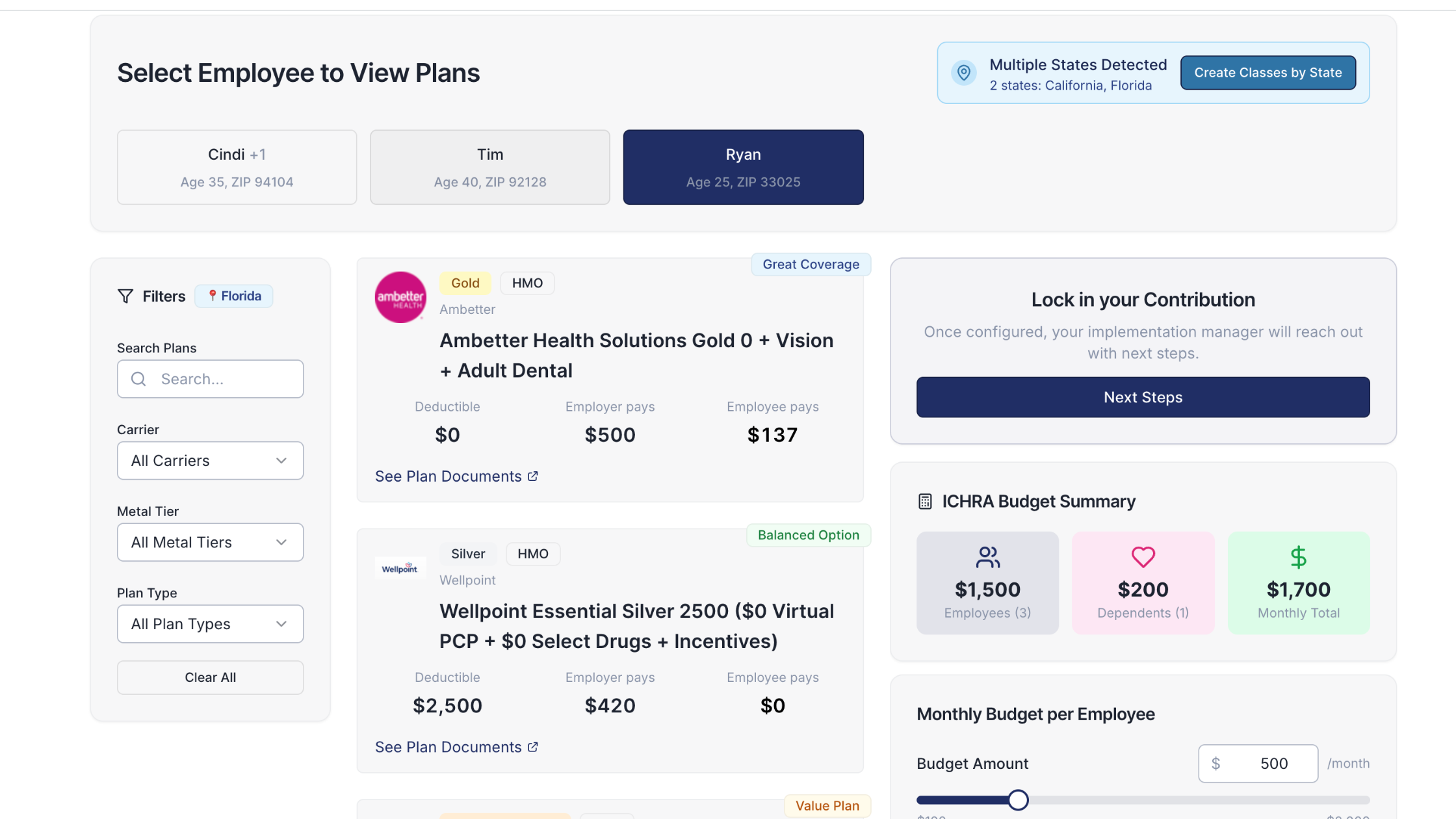
Simple, personalized health benefits
Sign up in minutes, define your contribution, and let your employees choose the health plan that works right for them
Integrations to make everything run smoothly
We'll connect with your payroll and finance systems to make deductions and premium payments seamless
Easy onboarding and off-boarding
In just a few clicks, add your roster and make updates on the fly. We'll handle it from there.
Venteur Certified Brokers to help your employees pick the right plan
Our trusted brokers ensure the best outcomes for employees and employers by unlocking health savings and providing unrivaled plan options.
AI-powered plan recommendations to give you confidence while you shop
Backed by 30 years of healthcare data, Venteur’s AI helps employees compare and choose the best plan for their unique situation.
Compliance and reporting because no-duh!
Venteur manages plan administration, reporting, and compliance so you can focus on growing your business.