Demystifying Health Reimbursement Arrangements: Your 2025 Guide
.avif)
Decoding Health Reimbursement Arrangements
Exploring the Features of HRAs
Let's start by uncovering the various features that make HRAs so intriguing. These arrangements offer employers a way to provide their employees with funds to cover eligible healthcare expenses. With HRAs, the financial burden of medical costs can be lifted off the shoulders of employees, making it a win-win situation for both parties.
But what exactly are the features that make HRAs stand out? One key feature is the flexibility they offer. HRAs can be customized to suit the unique needs of different organizations. Employers have the freedom to determine the amount of funds allocated to employees and the types of expenses that can be reimbursed. This personalized approach to healthcare benefits ensures that employees receive the support they need, while employers have control over their healthcare spending.
Furthermore, HRAs provide a tax advantage for both employers and employees. Contributions made by employers to HRAs are tax-deductible, reducing their overall tax liability. On the other hand, employees do not have to pay taxes on the funds they receive through HRAs, making it a valuable benefit.
What to Expect with an HRA: A Comprehensive Guide
So, you've heard about HRAs, and now you're curious about what you can expect as an employer or employee. In this section, we'll provide you with a step-by-step guide, walking you through the entire HRA journey.
First, let's talk about setting up an HRA plan. It involves several steps, such as determining the eligibility criteria for employees, establishing the funding amount, and selecting the types of expenses that will be covered.
Determining Eligibility for HRAs
HRAs can be offered to any employee or certain types of employees, based on specific job criteria. It's essential to ensure each class of employees is treated equally. Here's where it gets interesting:
- ICHRAs (Individual Coverage HRAs): Employees must have a qualified individual insurance plan to participate. This makes ICHRAs a flexible option for those who prefer individual plans over group coverage.
- QSEHRAs (Qualified Small Employer HRAs): Employees can either be covered by a spouse’s insurance plan or purchase their own qualified individual insurance. This provides versatility for small businesses looking to offer competitive benefits without a traditional group plan.
Regardless of the type, it's important to note that employees must have health insurance to participate in an HRA. Additionally, they cannot be simultaneously offered a group plan, ensuring there's no overlap in coverage.
By carefully considering these factors, you can design an HRA plan that aligns with your company's goals and meets the diverse needs of your workforce.
Once the HRA plan is in place, the next step is managing reimbursements. Employees will need to submit claims for eligible expenses, and employers will need to review and approve these claims. We'll explain how employees can submit claims, what documentation is required, and the timeframes for reimbursement. This comprehensive guide will equip you with all the necessary information to effectively manage HRAs and ensure a seamless experience for everyone involved.
Understanding HRA Administration
An HRA administrator plays a crucial role in the design and management of the arrangement. It's essential to engage a third-party administrator for several reasons, the most significant being privacy. This ensures compliance with the Health Insurance Portability and Accountability Act (HIPAA), as employees' medical expenses, including individual health insurance premiums, are considered Protected Health Information (PHI).
Compliance and Record Keeping
In addition to HIPAA compliance, maintaining adherence to IRS regulations is vital. HRAs offer tax advantages, so businesses must keep detailed records for up to seven years. This not only ensures compliance but also safeguards against potential audits.
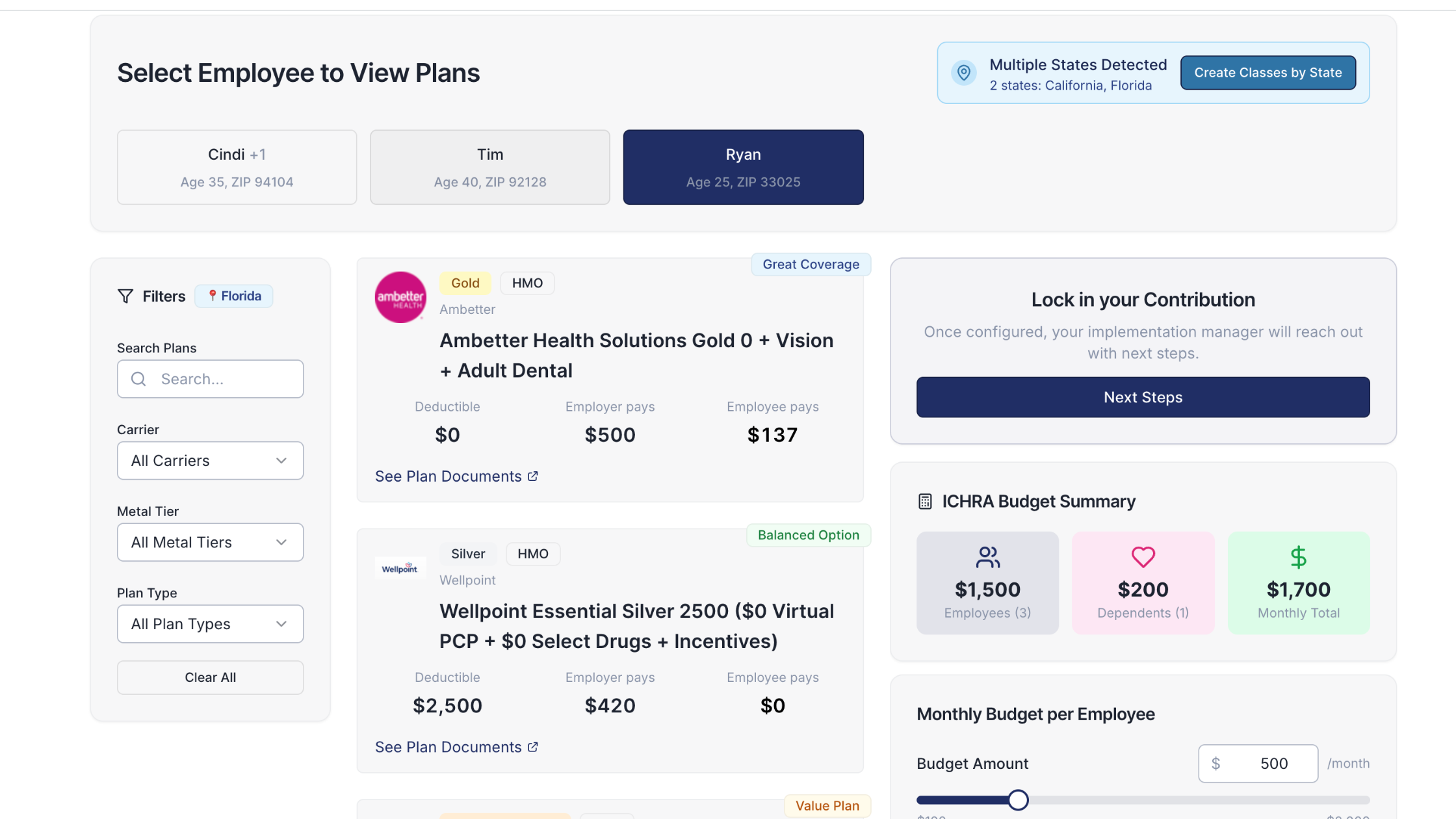
Streamlined HRA Plan Administration
Administering an HRA can be broken down into four straightforward steps:
- Design the HRA Plan: Employers start by crafting their HRA plan, considering the specific needs of their organization and employees.
- Employee Enrollment: Employees purchase their preferred health insurance plans. Guidance and resources are often available to assist employees in making informed choices.
- Claims Submission: Once employees have their plans, they can submit eligible reimbursement claims. Proper documentation, such as receipts, must accompany these claims for validation.
- Reimbursement: Employers review, approve, and reimburse employees for all valid claims, ensuring a smooth process.
Efficiency and Support
With the right tools and support, the administration can be efficient. Many organizations find that they spend minimal time each month on HRA administration, thanks to streamlined processes and expert guidance available from third-party administrators. For a more detailed explanation, additional resources are available to help tailor the plan to specific HRA types, such as QSEHRA or ICHRA.
By following these guidelines and leveraging expert assistance, managing an HRA becomes a manageable and efficient process, benefiting both employers and employees alike.
Understanding HRA Requirements
When it comes to Health Reimbursement Arrangements (HRAs), the requirements can differ based on the specific type of HRA you're considering. Let's explore the key distinctions between two popular types: Individual Coverage HRA (ICHRA) and Qualified Small Employer HRA (QSEHRA).
Individual Coverage HRA (ICHRA)
- Employer Size Flexibility: There are no restrictions on the size of the employer; organizations of any scale can offer an ICHRA to their employees.
- Group Health Plan Compatibility: Employers can offer both a group health plan and an ICHRA, but not to the same employee class. For instance, full-time employees might receive a group health plan, while part-time employees could be provided an ICHRA.
Qualified Small Employer HRA (QSEHRA)
- Employer Size Limitations: This option is specifically designed for small employers with less than 50 full-time employees. Employers beyond this size threshold do not qualify for offering QSEHRA.
- Group Health Plan Exclusivity: Unlike the ICHRA, employers offering a QSEHRA cannot provide any group health insurance plans. Moreover, QSEHRA does not allow for distinctions among employees based on class options, such as hours worked or geographical location.
These differences highlight the tailored nature of HRAs to meet various organizational needs while adhering to the stipulations outlined in relevant IRS regulations. Understanding these requirements ensures that employers choose the right type of HRA to suit both their size and strategic health benefit offerings.
Understanding Different Types of HRAs
HRAs come in various flavors, each with its own set of rules and regulations. It's time to put on your explorers' hat as we dive into the world of different HRA types.
One such type is the Individual Coverage HRA (ICHRA). This HRA allows employers to provide funds for employees to purchase individual health insurance plans. It's a great option for employers who want to offer more choice and flexibility to their employees. We'll explore the ins and outs of this HRA type, discussing its eligibility requirements, contribution limits, and how it stacks up against other options.
Another interesting option is the Qualified Small Employer HRA (QSEHRA). Designed specifically for small businesses, this HRA offers unique advantages. It allows small employers who do not offer group health insurance to provide tax-free funds to employees for medical expenses. We'll take a close look at the benefits it brings to the table and help you determine if it's the right fit for your organization.
Understanding QSEHRA Affordability
Determining the affordability of a Qualified Small Employer Health Reimbursement Arrangement (QSEHRA) involves a few key steps. Here's a breakdown of the process:
- Identify the Benchmark Plan: Begin with finding the least expensive silver plan available in the marketplace. This serves as the benchmark for calculating affordability.
- Calculate the Threshold: Next, assess the threshold where the reimbursement becomes affordable. To do this, multiply the employee’s household income by 9.83%. This percentage is used as a guideline, based on IRS regulations, for determining affordability.
- Compare the Contribution: Finally, the QSEHRA contribution offered by the employer should exceed the difference between the cost of the benchmark silver plan and the calculated threshold. If the contribution surpasses this difference, it can be considered affordable under QSEHRA rules.
By following these steps, employers can ensure that their QSEHRA offerings meet the necessary affordability criteria, helping employees access health coverage without undue financial strain.
But wait, there's more! HRAs have evolved over time, and there are other lesser-known HRA types that might just pique your interest. For example, the Excepted Benefit HRA (EBHRA) allows employers to provide additional funds for employees to cover dental and vision expenses. We'll explore these lesser-known HRA types, uncovering their unique features and potential benefits. Discovering new HRA possibilities and expanding your knowledge has never been more exciting!
Qualified Health Plans for QSEHRA
When considering the right health plans that qualify for a Qualified Small Employer Health Reimbursement Arrangement (QSEHRA), it's important to ensure they meet certain criteria specified by the IRS.
Eligible Plans
- Minimum Essential Coverage (MEC): Any health plan that satisfies the IRS's Minimum Essential Coverage standards is eligible. Here's a closer look at what types of plans fall under this category:
- Exchange-Based Plans: Bronze, Silver, and Gold plans available through the Health Insurance Marketplace.
- Government-Sponsored Plans: This includes Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP).
- Catastrophic Plans: Available for individuals under 30 or those qualifying for a hardship exemption. These plans typically have lower premiums but high deductibles.
- Student Health Plans: Insurance plans provided through educational institutions.
- Dependent Health Plans: Plans under a spouse’s or parent’s health insurance.
Ineligible Plans
While the above plans qualify, some do not meet the standards for a QSEHRA:
- Health Sharing Ministries: These plans often pool resources among members but do not qualify as insurance.
- Short-term Health Plans: Temporary plans designed to cover gaps in insurance.
- Indemnity Health Plans: These plans pay a set amount per service and do not meet MEC standards.
By understanding the qualifications and exclusions, small employers can better navigate the offerings available and make informed decisions for their health reimbursement arrangements.
What Are the Qualified Health Plans for ICHRA?
Understanding the types of health insurance plans that qualify for Individual Coverage Health Reimbursement Arrangements (ICHRA) is essential for making informed decisions. Here’s a breakdown of the eligible plans:
- Marketplace Health Plans: These include Bronze, Silver, and Gold tiers purchased through the health insurance exchange.
- Medicare Options: Coverage under Medicare Part A and B or a Medicare Advantage Plan (Part C) meets ICHRA requirements.
- Catastrophic Health Plans: Available to individuals under 30 or those who qualify for a hardship exemption, these plans are designed for unexpected, high-cost situations.
- Student Health Plans: Policies available to university students can also qualify for ICHRA reimbursements.
Important Exclusions
It's crucial to note that plans such as those offered through a spouse or parental coverage do not qualify for ICHRA. Always verify specific plan details with your insurance provider to ensure eligibility.
Weighing the Pros and Cons of HRAs
The Benefits of HRAs: What Employers Need to Know
Now that we've covered the fundamentals, it's time to dive deeper into the perks of HRAs for employers. Spoiler alert: there are plenty of them! From tax advantages to increased control over healthcare costs, HRAs offer a range of benefits.
With HRAs, employers can attract and retain top talent by offering competitive healthcare benefits. This can be a game-changer in today's competitive job market, where employees are increasingly prioritizing comprehensive health coverage. By providing HRAs, employers can demonstrate their commitment to employee well-being and stand out as an employer of choice.
But the benefits don't stop there. HRAs also provide employers with the opportunity to customize their healthcare offerings to meet the unique needs of their workforce. Whether it's offering different coverage options for different employee groups or tailoring benefits to specific demographics, HRAs allow employers to provide targeted and personalized healthcare solutions.
Furthermore, HRAs offer tax advantages for employers. Contributions made to HRAs are tax-deductible, which can result in significant savings for businesses. This additional financial flexibility can be reinvested into other areas of the company, such as employee training and development or business expansion.
Potential Drawbacks of HRAs: Considerations for Employers
It's not all sunshine and rainbows. As with any arrangement, HRAs come with their fair share of potential drawbacks. In this section, we'll shed light on some considerations that employers should keep in mind.
One potential drawback of HRAs is the administrative complexity they can introduce. Setting up and managing an HRA plan requires careful attention to detail and ongoing administrative tasks. From determining eligibility criteria to handling reimbursement requests, employers need to allocate resources and manpower to ensure the smooth operation of the HRA.
Cost management challenges can also arise with HRAs. While employers have more control over healthcare costs with HRAs, there is still the potential for unexpected expenses. Factors such as changes in healthcare utilization, medical inflation, and the cost of prescription drugs can impact the financial viability of an HRA plan. Employers must carefully analyze and monitor these costs to ensure the sustainability of their healthcare benefits program.
Another consideration is the impact of HRAs on eligibility for premium tax credits. Employees who participate in an HRA may be ineligible for premium tax credits when purchasing coverage through the Health Insurance Marketplace. This can be a significant factor for employees who rely on these credits to make healthcare more affordable. Employers should communicate this potential impact to their employees and provide guidance on how to navigate the options available to them.
A Brief History of HRAs: Evolution and Impact
Curious about how HRAs came to be? You're in for a treat! In this section, we'll take a trip down memory lane to explore the evolution of HRAs and their impact on the healthcare landscape.
HRAs have a fascinating backstory that dates back to the early 2000s. They were initially introduced as a result of IRS guidance, which allowed employers to provide tax-free reimbursements for qualified medical expenses. This marked a significant shift in the way employers could offer healthcare benefits to their employees.
However, it was the passage of the Affordable Care Act (ACA) in 2010 that brought about major changes to HRAs. The ACA introduced new regulations and requirements for employer-sponsored health plans, including HRAs. These changes aimed to enhance consumer protections and increase access to affordable healthcare coverage.
Under the ACA, certain types of HRAs were deemed non-compliant, leading to a decline in their popularity. However, subsequent legislative changes and regulatory guidance have expanded the use of HRAs once again. In 2019, the Trump administration issued a new rule that created two types of HRAs: the Individual Coverage HRA and the Excepted Benefit HRA. These new HRA options have opened up opportunities for employers to provide flexible and cost-effective healthcare benefits.
Today, HRAs continue to play a significant role in the healthcare landscape. They offer employers a versatile tool to navigate the complexities of providing healthcare benefits to their workforce. As healthcare needs and regulations evolve, HRAs are likely to adapt and innovate to meet the changing demands of employers and employees alike.
Demystifying HRA Plans: How Do They Work?
Now that you have a solid understanding of HRAs, it's time to dig even deeper and unravel the inner workings of HRA plans. In this section, we'll answer questions like:
- How do employers fund HRAs?
- What expenses are eligible for reimbursement?
- How do employees access their HRA funds?
Consider this section your HRA playbook, guiding you through the intricacies of HRA plans and ensuring you're well-equipped to navigate this exciting terrain.
Navigating Health Insurance Reimbursement for Employees
Are HRAs Considered Income? Understanding the Tax Implications
Money matters can be perplexing, especially when it comes to taxes. If you're wondering how HRAs impact your tax situation as an employee, we've got the answers you're seeking.
In this section, we'll address the million-dollar question: Are HRAs considered income? We'll delve into the tax implications of HRAs and provide valuable insights to help you navigate this financial maze with confidence.
HRAs vs. Health Insurance: Key Differences Explained
Health insurance and HRAs may seem similar, but they serve different purposes. In this section, we'll dissect the key differences between the two, helping you understand the unique advantages that HRAs bring to the table.
From coverage options to flexibility in healthcare choices, you'll discover why HRAs are not just a run-of-the-mill healthcare benefit. Prepare to have your mind blown as we paint a clear picture of how HRAs stand out in the crowd.
How Should Employees Be Educated About Using an HRA?
Educating employees about using a Health Reimbursement Arrangement (HRA) effectively involves a few key steps. Here’s a comprehensive approach to ensure employees understand and utilize their HRAs with confidence:
1. Start with the Basics
- Overview Session: Begin with an introductory meeting to explain what an HRA is and its benefits.
- Simple Definitions: Define key terms like "reimbursement," "eligible expenses," and "premium tax credits."
2. Detailed Workshops
- Reimbursement Process: Conduct workshops to walk through the reimbursement process step-by-step.
- Interactive Demos: Use role-playing or interactive scenarios to illustrate real-life applications.
3. Provide Comprehensive Materials
- Handouts and Guides: Distribute easy-to-understand materials that summarize HRA rules and procedures.
- FAQs: Develop a Frequently Asked Questions document to address common concerns and get ahead of potential confusion.
4. Utilize Technology and Tools
- Online Resources: Offer access to online portals and tools where employees can learn at their own pace.
- Webinars: Host regular webinars to provide updates or refreshers on how to use the HRA effectively.
5. Encourage Ongoing Support
- Q&A Sessions: Schedule regular Q&A sessions with HR or financial advisors.
- Feedback Mechanism: Encourage employees to provide feedback on the education process and areas where they need more clarity.
6. Highlight the Impact on Tax Credits
- Explain Tax Components: Clarify how HRAs interact with premium tax credits to prevent misunderstandings during tax season.
- Offer Scenarios: Provide examples that show different scenarios of using HRAs in conjunction with health plans and tax credits.
By implementing these strategies, employers can ensure their team is well-equipped to manage their health reimbursement arrangements, making the process smooth and efficient for everyone involved.
Unlocking the Power of HRA Funds: A Guide for Employees
As an employee, it's important to know how to leverage your HRA funds effectively.
Start by checking out our list of ICHRA eligible expenses which have been sourced from IRS Publication 502. Remember, HRAs are not just an acronym - they represent a world of possibilities and benefits for both employers and employees.
What Qualifies Under HRA Reimbursement?
To make the most of your HRA, it's crucial to understand what expenses qualify for reimbursement. Here's a quick guide:
- Qualified Medical Expenses: These include a wide range of health-related costs such as doctor visits, prescription medications, and medical equipment.
- Health Plans: You can also get reimbursed for health plans purchased through Healthcare.gov or state exchanges. This provides flexibility in choosing a plan that works best for you.
By familiarizing yourself with these categories, you can maximize the benefits of your HRA and enjoy greater financial flexibility.
So go forth, armed with your newfound knowledge, and embrace the power of HRAs in 2025 and beyond!
You got questions, we got answers!
We're here to help you make informed decisions on health insurance for you and your family. Check out our FAQs or contact us if you have any additional questions.
Explore more related content
What is Venteur
Explore the best human-first Health Insurance platform
Simple, personalized health benefits
Sign up in minutes, define your contribution, and let your employees choose the health plan that works right for them
Integrations to make everything run smoothly
We'll connect with your payroll and finance systems to make deductions and premium payments seamless
Easy onboarding and off-boarding
In just a few clicks, add your roster and make updates on the fly. We'll handle it from there.
Venteur Certified Brokers to help your employees pick the right plan
Our trusted brokers ensure the best outcomes for employees and employers by unlocking health savings and providing unrivaled plan options.
AI-powered plan recommendations to give you confidence while you shop
Backed by 30 years of healthcare data, Venteur’s AI helps employees compare and choose the best plan for their unique situation.
Compliance and reporting because no-duh!
Venteur manages plan administration, reporting, and compliance so you can focus on growing your business.