Advanced Premium Tax Credits (APTCs): A Comprehensive Guide

Imagine being able to reduce your health insurance costs drastically. APTCs are the hidden lifeline that makes quality healthcare affordable for millions of Americans struggling to manage rising medical expenses. These tax credits are more than just financial assistance—they're a critical bridge that helps lower-income families access essential health coverage, transforming what could be an overwhelming economic burden into a manageable monthly expense. While the system may seem complex, APTCs offer a powerful solution to one of the most pressing challenges in healthcare: making medical coverage accessible to those who need it most.
What are Advanced Premium Tax Credits?
Chances are that you’ve heard of “Obamacare.” Advanced Premium Tax Credits or “APTCs” are the formal name of “Obamacare Subsidies.”
APTCs provide financial assistance to lower-income individuals and families to reduce their monthly health insurance premiums. Unlike traditional tax credits, these are applied directly to your monthly insurance bill.
How do APTCs Work?
When a consumer applies for health insurance through Healthcare.gov, the Marketplace will:
- Estimate the amount of Premium Tax Credits (PTC) the consumer can claim
- Calculate the credit based on:
- Individual/family income
- Age
- Household size
- Local plan costs
Consumers can choose to:
- Apply all estimated credits to lower monthly premiums
- Apply some credits
- Decline advanced credits entirely
Their estimated PTC paid their health insurance company in advance to lower their monthly premiums—hence the term Advanced Premium Tax Credit.
Annual Reconciliation During Tax Season
APTCs are reconciled annually during tax season. The IRS compares the APTCs received with the consumer's actual annual income when they file their taxes. This process can result in:
- Receipt of additional tax credits if you received less than you qualified for
- Potential repayment if you received more credits than your income justified
The exact repayment depends on the specific income difference and your individual circumstances. For individuals making less than 200% of the Federal Poverty Level (FPL), the maximum repayment is $350 (for tax year 2024). This amount increases for individuals with higher income:
- Income 200-300% of FPLl: $350
- Income 300-400% of FPL: $750
- Income 400%+ of FPL: Full amount of excess credits
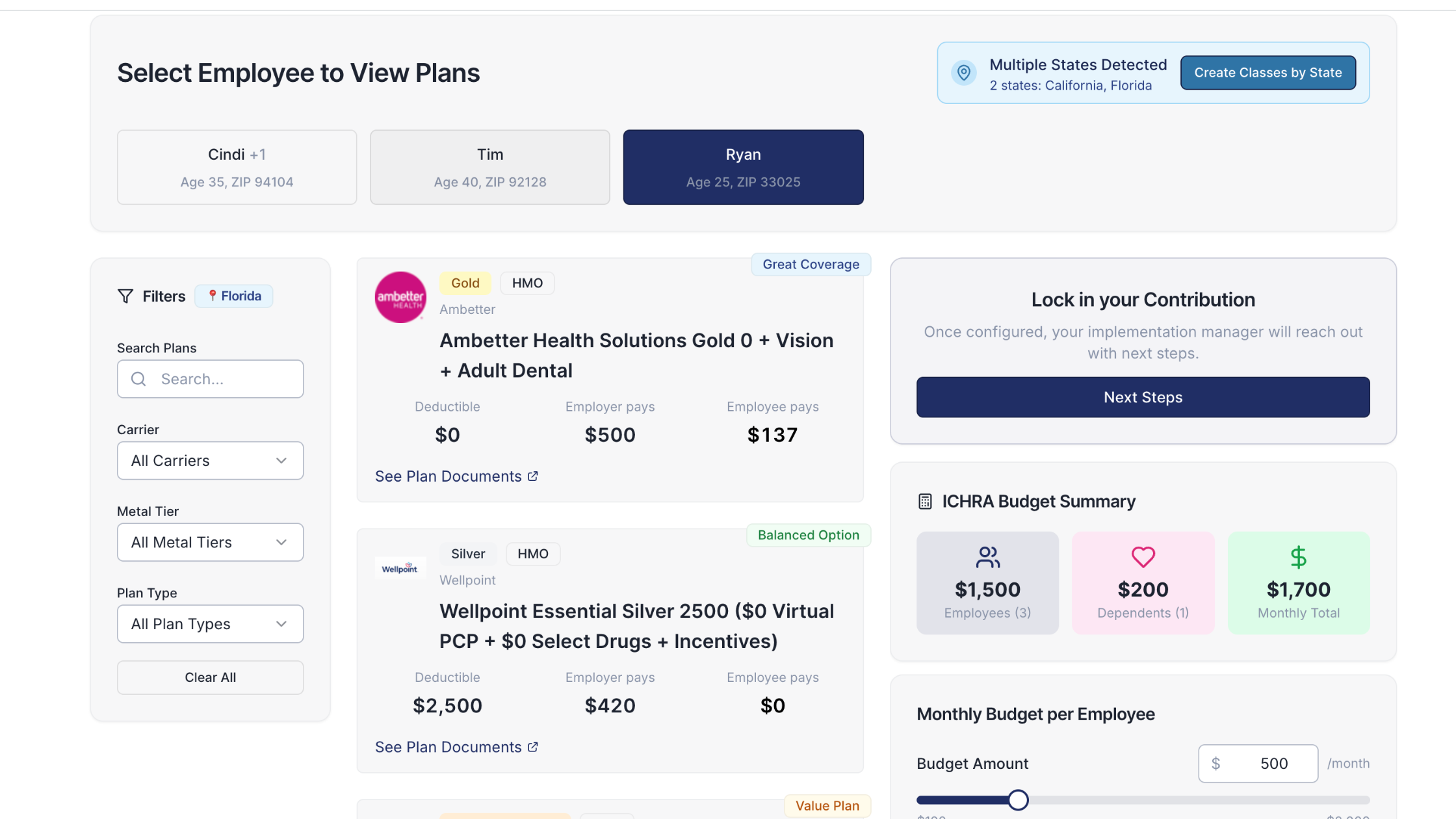
APTCs and Individual Coverage Health Reimbursement Arrangements (ICHRAs)
Individuals receiving an Individual Coverage Health Reimbursement Arrangement (ICHRA) from their employer face unique considerations regarding APTCS.
If an employer offers an ICHRA that is considered "affordable" under ACA guidelines, employees are ineligible for APTCs. The affordability is determined by comparing the ICHRA contribution to the employee's expected cost of the lowest-cost on-exchange silver plan. In 2024, the employee’s share of their health insurance premium cannot exceed 8.39% of their annual income in order for the ICHRA to be considered affordable. In 2025, the affordability threshold is 9.02%.
Employees who receive an ICHRA and claim APTCs are typically required to repay the tax credits in full.
Important Considerations
- Tax credit eligibility changes annually
- Consult a tax professional for personalized advice
- Visit HealthCare.gov for the most current information
You got questions, we got answers!
We're here to help you make informed decisions on health insurance for you and your family. Check out our FAQs or contact us if you have any additional questions.
Explore more related content
What is Venteur
Explore the best human-first Health Insurance platform
Simple, personalized health benefits
Sign up in minutes, define your contribution, and let your employees choose the health plan that works right for them
Integrations to make everything run smoothly
We'll connect with your payroll and finance systems to make deductions and premium payments seamless
Easy onboarding and off-boarding
In just a few clicks, add your roster and make updates on the fly. We'll handle it from there.
Venteur Certified Brokers to help your employees pick the right plan
Our trusted brokers ensure the best outcomes for employees and employers by unlocking health savings and providing unrivaled plan options.
AI-powered plan recommendations to give you confidence while you shop
Backed by 30 years of healthcare data, Venteur’s AI helps employees compare and choose the best plan for their unique situation.
Compliance and reporting because no-duh!
Venteur manages plan administration, reporting, and compliance so you can focus on growing your business.