A Comprehensive Guide to Section 111 Reporting for Employers Offering ICHRA Plans

If you’re an employer or a broker helping businesses with health benefits, you might have heard about something called an ICHRA. It’s a way for employers to help their employees pay for health insurance and qualified medical expenses. It also reimburses Medicare. This guide walks you through important rules you need to know specifically about Medicare reporting.
What is an ICHRA?
An ICHRA is a type of Health Reimbursement Arrangement (HRA) that allows employers to reimburse employees for qualified medical expenses, including premiums for individual health insurance. This flexible approach enables employers to tailor their health benefits to meet the diverse needs of their workforce.
The Medicare Part D Credible Coverage Notice
Under 42 CFR § 423.56, all group health plans, including ICHRAs, are subject to the Medicare Part D notice and disclosure requirements.
ICHRAs constitute non-creditable coverage under Medicare Part D when evaluated as standalone arrangements. Why? ICHRAs don't automatically include prescription drug coverage as a built-in feature. Unlike some health plans that come with prescription coverage already included, ICHRAs are just reimbursement accounts that employees use to purchase their own health insurance. The prescription drug coverage would depend entirely on which plan the employee chooses to buy with their ICHRA funds.
This means that if your ICHRA is available to employees who may be eligible for Medicare, you must provide them with a Notice of Credible Coverage.
Key Points:
- Employers must inform eligible participants whether their ICHRA is considered “creditable” coverage under Medicare Part D. (ICHRAs represent "non-creditable"coverage.)
- Send out this notice every year and whenever someone becomes eligible for Medicare.
Section 111 Reporting: What You Need to Know
Medicare Section 111 reporting is part of the Medicare Secondary Payer (MSP) requirements, which mandate reporting of certain information related to group health plan (GHP) arrangements, including ICHRAs.
Who is Responsible?
The “responsible reporting entity” is typically the Third-Party Administrator (TPA) managing the ICHRA (if you are our client, this means Venteur). They submit required information to the Centers for Medicare & Medicaid Services (CMS) concerning ICHRA participants enrolled in Medicare.
Quarterly Reporting Requirements:
Annual Benefit Amount: If an employee’s ICHRA has benefits of $5,000 or more, the TPA must report it. If it’s less than $5,000, they don’t need to report it.
Termination Date: If an employee stops using the ICHRA or runs out of benefits, the TPA needs to report when that happened. If the ICHRA is still active each year, they will report that it’s ongoing.
Types of Coverage: If the ICHRA helps with both medical care and prescription drugs, the TPA has to send in two separate reports for that employee.
Compliance Steps for Employers
Talk to Your TPA: Make sure your TPA knows about their reporting duties and is ready to submit the required information every three months.
Help Employees Understand: Explain to your employees about the Medicare notice and make sure they get it on time.
Keep Track of Benefits: Make sure you know how much each employee is getting from their ICHRA so the right information gets reported.
Check Your ICHRA Plan: Review your plan annually to make sure it follows all the rules and meets your employees' needs.
Additional Resources
For further details on the Medicare Section 111 reporting requirements, the MMSEA Section 111 MSP Mandatory Reporting GHP User Guide, Version 7.2 provides comprehensive instruction.
You got questions, we got answers!
We're here to help you make informed decisions on health insurance for you and your family. Check out our FAQs or contact us if you have any additional questions.
Explore more related content
What is Venteur
Explore the best human-first Health Insurance platform
Simple, personalized health benefits
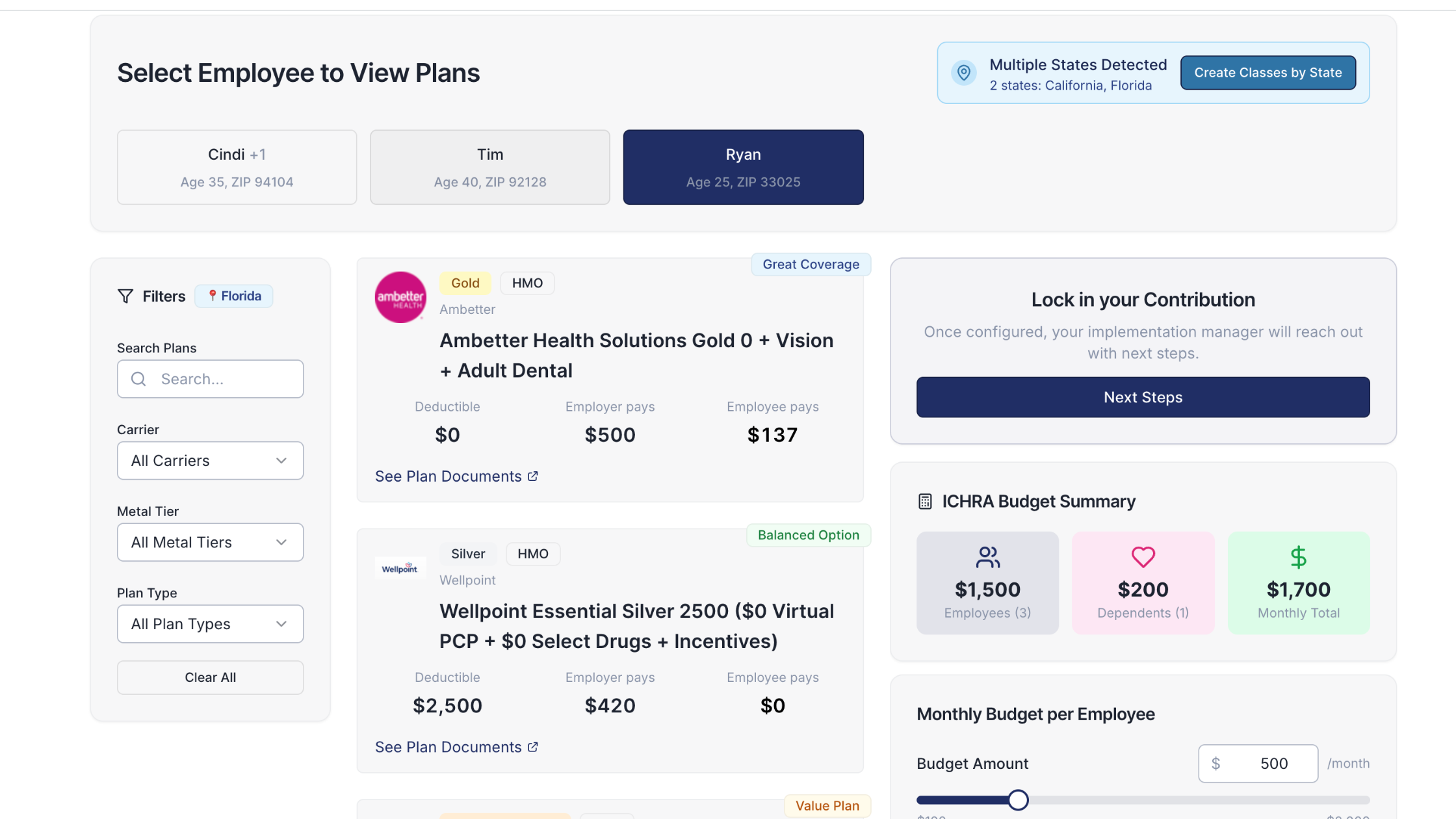
Sign up in minutes, define your contribution, and let your employees choose the health plan that works right for them
Integrations to make everything run smoothly
We'll connect with your payroll and finance systems to make deductions and premium payments seamless
Easy onboarding and off-boarding
In just a few clicks, add your roster and make updates on the fly. We'll handle it from there.
Venteur Certified Brokers to help your employees pick the right plan
Our trusted brokers ensure the best outcomes for employees and employers by unlocking health savings and providing unrivaled plan options.
AI-powered plan recommendations to give you confidence while you shop
Backed by 30 years of healthcare data, Venteur’s AI helps employees compare and choose the best plan for their unique situation.
Compliance and reporting because no-duh!
Venteur manages plan administration, reporting, and compliance so you can focus on growing your business.