Health Insurance Acronyms Explained

TL;DR:
- There are 2,000+ health plans available to ICHRA consumers, each with its own benefits and limitations.
- Understanding health insurance acronyms (premiums, deductibles, copayments, out-of-pocket maximums, HMO, PPO, EPO, POS, PCPs, specialists, RNs, LPNs, and PTs) can help you make informed decisions.
- Building your health insurance literacy is important for your health and financial well-being.
Acronyms for Health Insurance Costs
Let's start by exploring the concept of premiums. A premium is the amount of money you pay to your insurance provider on a regular basis, typically monthly or annually. It's essentially the cost of having insurance. Understanding how premiums are calculated can help you make informed decisions when choosing a plan that fits your budget.
Next up, deductibles. A deductible is the amount of money you must pay out of pocket before your insurance coverage kicks in. It's important to note that deductibles can vary depending on the type of plan you have. Some plans have high deductibles, so you'll have to pay a significant amount before your insurance starts covering your medical expenses. Other plans have lower deductibles, making it easier to reach the coverage threshold.
Now, let's talk about copayments. A copayment, or copay, is a fixed amount you pay for specific services or medications. For example, you may have a $20 copay for a doctor's visit or a $10 copay for a prescription. Copayments are typically due at the time of service and can vary depending on the healthcare provider or the medication type.
Another important term to understand is the out-of-pocket maximum. This term refers to the maximum amount you'll pay for covered services annually. Once you reach this threshold, your insurance will cover 100% of the costs for the remainder of the year. Knowing your out-of-pocket maximum can provide peace of mind, as it sets a limit on your potential financial liability.
What Does OOP Mean in Health Insurance Terms?
In the context of health insurance, "OOP" stands for "out-of-pocket." This term refers to the expenses that you personally cover for medical services that are not reimbursed by your insurance provider. Understanding OOP costs is crucial because it directly impacts your budget and healthcare affordability.
Key Components of Out-of-Pocket Costs:
- Deductibles: The initial amount you pay for health services before your insurance starts covering expenses.
- Copayments: Set fees you pay for specific services, such as doctor's visits or prescriptions.
- Coinsurance: The percentage of costs you cover after meeting your deductible.
- Out-of-Pocket Maximum: The maximum limit on the costs you will pay during a policy period, after which your insurance covers additional expenses fully.
It's essential to be familiar with each of these elements to gauge how much you'll need to allocate from your own funds for healthcare beyond what your insurance plan covers. Understanding OOP can help you plan financially and make informed decisions about your health insurance plan options.
Acronyms Related to Health Insurance Plans
When it comes to health insurance plans, things can get pretty acronym-heavy. It's like learning a new language! But fear not, we're here to help you understand the different types of plans available.
Let's start with HMO, which stands for Health Maintenance Organization. This type of plan typically requires you to choose a primary care physician who will coordinate your healthcare and refer you to specialists when needed.
Another common acronym is PPO, which stands for Preferred Provider Organization. With a PPO plan, you have more flexibility in choosing healthcare providers. You can see specialists without a referral, but you'll pay less if you stay within the network of preferred providers.
Next up is EPO, which stands for Exclusive Provider Organization. Like a PPO, an EPO plan allows you to see specialists without a referral. However, you must stay within the network of providers to receive coverage.
We also have POS, which stands for Point of Service. This type of plan combines elements of both HMO and PPO plans. You'll need to choose a primary care physician, but you can also see specialists outside the network with a referral.
Finally, ESI stands for Employer-Sponsored Insurance. This type of health insurance is provided by companies as a benefit to their employees. It's a common perk offered by many businesses, such as Google and Amazon, to attract and retain talent.
What Does It Offer?
- Coverage: ESI typically includes medical, dental, and vision plans.
- Cost-sharing: Employers often pay a portion of the premium, making it more affordable for employees.
- Access: Employees gain access to a network of healthcare providers.
Who Provides ESI?
- Employers: Companies ranging from small businesses to multinational corporations.
- Insurers: Providers like UnitedHealthcare and Blue Cross Blue Shield partner with companies to offer these plans.
In essence, ESI is a strategic advantage for businesses and a valuable asset for employees.
What Qualifies a Health Plan as a QHP under the ACA?
A Qualified Health Plan (QHP) is a specific type of health insurance policy that complies with standards set by the Affordable Care Act (ACA). Here's what makes a health plan eligible for this designation:
- Compliance with ACA Requirements
- To qualify as a QHP, the plan must adhere to numerous stipulations detailed in the ACA. These include providing essential health benefits across ten categories such as emergency services, maternity care, and prescription drugs.
- Marketplace Certification
- The plan must be certified by the Health Insurance Marketplace, ensuring it meets established benchmarks, including adequate coverage levels and provider networks.
- Affordable Premiums and Cost-Sharing
- A QHP must offer premiums and cost-sharing options (like deductibles and co-payments) that align with ACA guidelines. This ensures healthcare is both accessible and affordable to consumers.
- Quality Standards
- The plan must meet quality standards, which are regularly assessed to ensure that consumers receive effective and efficient care. This includes patient experience and outcomes.
- Provider Network Adequacy
- It must maintain a network of healthcare providers that is sufficient to cover its enrollees without causing undue delays in obtaining treatment or services.
By conforming to these comprehensive criteria, a health plan earns its status as a QHP, ensuring it offers consumers robust protection and value aligned with national healthcare reforms.
Acronyms Associated with Health Care Providers
Now, let's shine a light on the acronyms that refer to different types of healthcare providers so you'll know who's providing your care.
First, we have PCP, which stands for Primary Care Physician. Your PCP is your main point of contact for all your healthcare needs. They provide preventive care, diagnose and treat common illnesses, and refer you to specialists when necessary.
Next, we have specialists. Specialists are doctors with expertise in specific areas of medicine. You may come across acronyms like ENT (Ear, Nose, and Throat), OB/GYN (Obstetrician/Gynecologist), or Cardiologist (specializes in heart-related conditions).
Other healthcare providers you may encounter include RNs (registered nurses), LPNs (Licensed Practical Nurses), and PTs (Physical Therapists). Each of these providers plays a crucial role in delivering quality care.
The ED, short for Emergency Department, is a critical section of hospitals dedicated to providing immediate care for patients facing urgent medical situations. It's often referred to as the ER, which stands for Emergency Room.
ABA, or Applied Behavior Analysis, is a therapeutic approach commonly covered by health insurance plans. It's primarily aimed at assisting individuals with autism and other developmental disorders. This therapy emphasizes analyzing and modifying behavior patterns to enhance one's social interaction, communication abilities, and learning proficiency.
An Ambulatory Surgery Center (ASC) is a specialized healthcare facility where patients can undergo surgical procedures that don't require an overnight hospital stay. These centers focus on providing a wide range of outpatient surgeries, offering a more convenient and often cost-effective alternative to hospital-based surgeries.
Finally, OTC stands for Over-the-Counter. This term is used to describe medications and health products that you can purchase without a prescription from a healthcare provider. These products are readily available in pharmacies, grocery stores, and even online. The convenience of OTC items makes them popular for treating common ailments, such as headaches, colds, and allergies.
These terms all point to the same essential function: delivering rapid and effective care when it's needed most.
Understanding Essential Health Benefits (EHBs) and Their Link to the ACA
Essential Health Benefits (EHBs) refer to a comprehensive set of healthcare services that insurance plans must offer under the Affordable Care Act (ACA). These benefits are mandated to ensure that individuals and families receive necessary healthcare coverage without being burdened by excessive out-of-pocket costs.
Key Aspects of EHBs:
- Broad Coverage: EHBs encompass a wide range of services. This includes inpatient and outpatient care, mental health services, prescription drugs, maternity and newborn care, and preventive services among others.
- Standardization Across Plans: The ACA requires all insurance plans, particularly those available in the Health Insurance Marketplace, to cover these benefits. This standardization helps consumers compare plans knowing they all offer the same basic benefits.
- Consumer Protection: By mandating these benefits, the ACA aims to prevent insurers from offering subpar plans that could leave consumers vulnerable in critical health situations.
Connection to the Affordable Care Act
The ACA, implemented in 2010, revolutionized healthcare by making it more accessible and affordable. One of its key provisions is the inclusion of EHBs in all new health insurance plans offered on the Marketplace. This requirement ensures that policies cannot omit crucial benefits, thus protecting consumers and promoting comprehensive health coverage.
By linking EHBs to the ACA, the legislation supports a minimum standard of care that must be met across all states, though states can have some flexibility to tailor specific aspects.
In essence, EHBs are a cornerstone of the ACA's mission to create a fairer and more inclusive healthcare system, ensuring broader access to essential medical services.
What is HIPAA, and What is Its Purpose in Healthcare?
HIPAA stands for the Health Insurance Portability and Accountability Act, a significant U.S. Law enacted in 1996. Its primary aim is to safeguard patients' private health information and ensure confidentiality in the healthcare sector.
Key Objectives of HIPAA:
- Privacy Protection: One of HIPAA's core purposes is to protect sensitive patient health information from being disclosed without the patient's consent or knowledge. This includes any information that can be used to identify an individual, such as medical records and personal health details.
- Security Standards: HIPAA mandates specific security measures that healthcare providers must implement to ensure the safety of electronic health information. This includes requiring strong data encryption and access controls to prevent unauthorized access.
- Portability: Another essential aspect of HIPAA is facilitating the transfer of health insurance information for individuals who change or lose their jobs, ensuring continuous health coverage.
- Administrative Simplification: By establishing standardized electronic transmission of administrative and financial transactions, HIPAA aims to reduce healthcare costs.
- Fraud Prevention: The act also includes provisions to combat healthcare fraud and abuse, promoting the integrity of the healthcare system.
In essence, HIPAA is crucial because it helps maintain trust between patients and healthcare providers by ensuring that private health details remain secure and confidential.
Understanding QLEs and Their Impact on Health Insurance Enrollment
A Qualifying Life Event (QLE) is a significant change in your life that can have a direct impact on your health insurance needs. Events such as marriage, childbirth, or losing other health coverage open up a unique opportunity in the insurance landscape.
What Happens After a QLE?
When a QLE occurs, it triggers a Special Enrollment Period (SPE). This period is a designated timeframe that allows you to sign up for or modify your health insurance plan, even if it's outside the usual open enrollment window. Typically, the open enrollment period runs from November 1 through December 15, but a QLE grants you a chance to adjust your policy beyond these dates.
Key Points to Remember:
- Examples of QLEs: Changes in marital status, birth or adoption of a child, or job loss.
- SPE Duration: Generally lasts 60 days from the date of the event.
- Eligibility: You can enroll in a new plan or make changes to your existing policy.
Having a clear understanding of QLEs is crucial for maintaining appropriate coverage and avoiding potential gaps during unexpected life changes. Whenever a life event significantly alters your circumstances, don't overlook the opportunity to evaluate and update your insurance options.
Understanding SEPs in Health Insurance
A SEP or Special Enrollment Period, is a designated timeframe that allows individuals to sign up for or modify their health insurance plans outside the usual open enrollment period. This opportunity arises under specific circumstances known as qualifying life events (QLEs).
What Triggers a Special Enrollment Period?
Special Enrollment Periods can occur after a range of life changes. These qualifying events might include:
- Marriage or Divorce
- Birth or Adoption of a Child
- Loss of Other Health Coverage, such as losing a job
- Relocation to a New Area, affecting your plan options
The exact time you have to enroll during an SPE can vary, but it typically ranges from 30 to 60 days following the qualifying event. It's crucial to act swiftly to ensure continuous health coverage and avoid potential penalties.
What is the Role of the IRS, HHS, and FDA in Relation to Health Insurance?
The Internal Revenue Service (IRS), the federal agency tasked with enforcing tax regulations, plays a pivotal role in the realm of health insurance. Its responsibilities extend beyond traditional tax collection duties. Here's how the IRS is involved:
- Tax Credits and Deductions
The IRS oversees the administration of health insurance-related tax credits, such as the Premium Tax Credit. This credit assists eligible individuals in reducing the cost of health insurance purchased through the Health Insurance Marketplace. - Tax Reporting and Compliance
It requires individuals and employers to report their health insurance coverage status. This ensures compliance with the Affordable Care Act (ACA) mandates, which include the provision of minimum essential coverage. - Penalties for Non-compliance
For those who fail to acquire necessary health insurance and do not qualify for an exemption, the IRS imposes penalties. This enforces ACA requirements and encourages individuals to obtain coverage. - Employer Mandate Enforcement
The IRS monitors large employers regarding the provision of affordable health insurance to employees. Failure to provide adequate coverage can lead to penalties, as outlined in the ACA.
Through these mechanisms, the IRS supports the broader objective of expanding access to health insurance and maintaining compliance with federal healthcare laws.
The Department of Health and Human Services (HHS) plays a crucial role in maintaining and enhancing public health in the United States. As a federal agency, HHS is responsible for implementing programs that focus on safeguarding citizens’ health and well-being.
Primary Responsibilities
- Healthcare Access: Ensures that people across the nation have access to essential medical services.
- Disease Prevention: Develops and promotes initiatives to prevent illness and control outbreaks.
- Research and Innovation: Supports medical research through agencies like the National Institutes of Health (NIH) to advance healthcare solutions.
Program Oversight
- Medicare and Medicaid: Administers these vital programs to assist vulnerable populations, including the elderly and low-income families.
- Public Health Safety: Enforces regulations and guidelines to protect the public from health threats.
By guiding public health policy and managing significant healthcare initiatives, HHS stands as a pillar of public health management in the United States.
The Food and Drug Administration (FDA) is a key player in the U.S. Healthcare system, acting as the regulatory backbone for a wide range of products. This government agency ensures that food, medicines, and medical devices are safe and effective for consumer use.
Key Responsibilities:
- Medication and Vaccine Approval: The FDA evaluates clinical trial data to determine whether new pharmaceuticals and vaccines are safe for public use. Only after a thorough review can these products enter the market.
- Safety Standards: It sets and enforces standards for food safety, cosmetic safety, and the efficacy of medical devices, ensuring consumer protection from harmful or ineffective products.
- Monitors Adverse Events: Once products are in the market, the FDA continues to monitor their performance through adverse event reporting systems, which can lead to further investigations or recalls if necessary.
- Labeling and Marketing: The agency also ensures that labels on food and drugs are accurate, providing consumers with essential information regarding ingredients, dosages, and potential side effects.
By maintaining these regulations and oversight, the FDA plays a crucial role in advancing public health. Its vigilant monitoring and evaluation processes help protect and improve the quality of life for millions of Americans.
Understanding the ACA and Its Impact on Health Insurance
The term ACA stands for the Affordable Care Act, a pivotal piece of legislation in the United States healthcare landscape. Often referred to as "Obamacare," this act was designed to enhance access to health insurance for millions of Americans.
Significance of the Affordable Care Act
- Creation of a Marketplace: The ACA established a federal health insurance marketplace, providing a platform where individuals and families can compare and purchase health insurance plans. This marketplace increased transparency and competition among insurers.
- Expansion of Coverage: The legislation significantly extended coverage by mandating insurance providers to offer insurance without denying coverage based on pre-existing conditions. It also expanded Medicaid eligibility in many states, allowing more low-income individuals and families to receive health coverage.
- Essential Health Benefits: The ACA required all insurance plans to cover a set of essential health benefits, such as emergency services, maternity care, mental health services, and prescription drugs, ensuring that comprehensive care is available to all insured individuals.
- Insurance Mandate: At its inception, the ACA included an individual mandate, which required most Americans to have health insurance or face a tax penalty. This mandate aimed to ensure a balanced risk pool, keeping insurance premiums affordable.
By laying this groundwork, the Affordable Care Act played a critical role in reshaping health insurance in the U.S., making it more accessible and comprehensive for a broad segment of the population.
What is an HRA, and How Does It Benefit Employees?
A Health Reimbursement Arrangement (HRA) is an employer-funded benefit plan designed to cover employees' out-of-pocket healthcare expenses. This arrangement allows employees to be reimbursed for qualified medical costs, making healthcare more affordable and accessible.
Key Features of an HRA:
- Employer-Funded: Unlike Health Savings Accounts (HSAs), only the employer contributes to an HRA. Employees don’t need to allocate any of their salary to benefit from this plan.
- Reimbursement for Medical Expenses: Employees can use HRA funds to cover a wide range of medical expenses. This can include co-pays, prescription medications, and various treatments.
- Tax Advantages: HRAs offer tax benefits for both employers and employees. Employers can deduct payments as a business expense, while employees enjoy tax-free reimbursements.
- Flexibility: Employers can tailor the plan to align with their business needs, such as rolling over unused funds or setting specific reimbursement categories.
Benefits for Employees:
- Reduced Financial Burden: HRAs alleviate the financial stress associated with healthcare costs by covering expenses that traditional insurance might not.
- Encouragement of Preventative Care: With out-of-pocket costs mitigated, employees may be more inclined to pursue preventative healthcare services, leading to better overall health.
- Increased Healthcare Choices: Employees have the flexibility to choose healthcare providers and services that meet their personal and family needs, without being restricted by network limitations.
Overall, HRAs provide valuable assistance in managing healthcare expenses, which can lead to improved employee satisfaction and well-being. By understanding HRAs, employees are empowered to make more informed healthcare decisions and enjoy a more comprehensive benefits package.
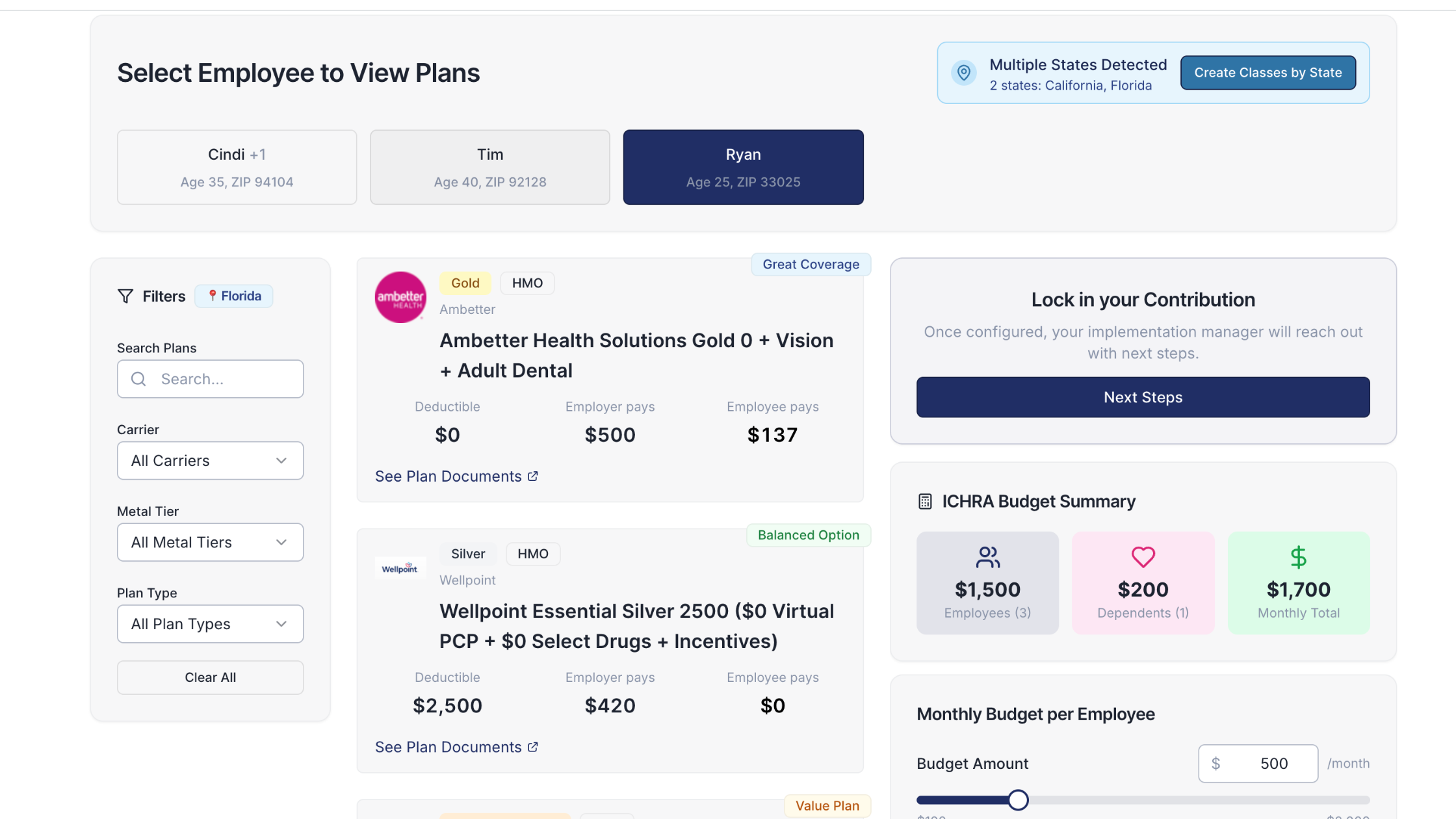
How ICHRA Works
- Employer Contribution: Employers set aside a designated amount of money on a pre-tax basis for each employee. This contribution can vary based on factors such as the employee's family size or geographic location.
- Employee Choice: Employees use these funds to buy health insurance through the individual market, which includes options from major providers like Blue Cross Blue Shield, UnitedHealthcare, and Kaiser Permanente.
- Flexibility and Personalization: This system allows employees to pick insurance plans that suit their personal or family circumstances, offering a level of customization not typically available in traditional employer-sponsored group health plans.
- Tax Advantages: Both employers and employees benefit from tax savings. Employers deduct the contributions from their business taxes, and employees receive funds without it being considered taxable income.
By shifting to ICHRA, companies provide employees with greater control over their health insurance while managing their healthcare benefits budget more effectively.
Understanding QSEHRA: A Brief Overview
A Qualified Small Employer Health Reimbursement Arrangement (QSEHRA) is a health benefit designed specifically for small businesses. It allows employers to reimburse their employees for medical expenses and individual health insurance premiums. This type of arrangement offers flexibility to smaller companies that may not be able to provide traditional group health insurance.
Key Features of QSEHRA:
- Annual Limitations:
- Employers can decide how much to reimburse, but there are federal limits set on the maximum annual contribution per employee. These limits vary based on whether the employee has a family or individual coverage plan.
- Employee Flexibility:
- Employees have the freedom to choose their healthcare plans based on their specific needs, which can then be reimbursed up to the employer-determined limits.
How QSEHRA Differs from ICHRA
While both QSEHRA and ICHRA (Individual Coverage Health Reimbursement Arrangement) serve similar purposes in reimbursing health costs, they differ significantly in their scope and limitations.
Differences:
- Scalability:
- QSEHRA is exclusively available to small employers with fewer than 50 full-time employees. It’s designed to support these smaller businesses in offering health benefits.
- ICHRA, on the other hand, is more versatile and can be offered by employers of any size, making it an option for both small and large businesses.
- Contribution Flexibility:
- QSEHRA has strict annual limits on how much can be reimbursed per employee, which are determined by the IRS each year.
- ICHRA allows employers more flexibility in terms of contributions, as there are no maximum contribution limits set by the IRS. Employers can tailor contributions based on different employee classes.
- Integration with Other Benefits:
- QSEHRA does not allow integration with any group health insurance plans.
- ICHRA, in contrast, can be offered alongside group health plans, providing a more comprehensive health benefit strategy.
By understanding these distinctions, small businesses can better decide which arrangement aligns with their goals and the needs of their employees.
Making Informed Health Insurance Decisions
Whether you're a health insurance newbie or a seasoned policyholder looking to expand your knowledge, this brief glossary is here to help. Check our blog regularly for more tips and tricks to help you build your health insurance literacy.
You got questions, we got answers!
We're here to help you make informed decisions on health insurance for you and your family. Check out our FAQs or contact us if you have any additional questions.
Explore more related content
What is Venteur
Explore the best human-first Health Insurance platform
Simple, personalized health benefits
Sign up in minutes, define your contribution, and let your employees choose the health plan that works right for them
Integrations to make everything run smoothly
We'll connect with your payroll and finance systems to make deductions and premium payments seamless
Easy onboarding and off-boarding
In just a few clicks, add your roster and make updates on the fly. We'll handle it from there.
Venteur Certified Brokers to help your employees pick the right plan
Our trusted brokers ensure the best outcomes for employees and employers by unlocking health savings and providing unrivaled plan options.
AI-powered plan recommendations to give you confidence while you shop
Backed by 30 years of healthcare data, Venteur’s AI helps employees compare and choose the best plan for their unique situation.
Compliance and reporting because no-duh!
Venteur manages plan administration, reporting, and compliance so you can focus on growing your business.